Amyotrophic Lateral Sclerosis (ALS) is a progressive neurodegenerative disease affecting nerve cells in the brain and in the spinal cord. As the disease progresses voluntary muscle action is severely compromised and the disease may cause total paralysis in its late stages.
Some genetic mutations can lead to inherited ALS, while patients with the non-inherited form of ALS display higher than normal levels of glutamate around the nerve cells in their spinal fluid. Glutamate is a chemical messenger in the brain. This chemical imbalance in the body, with glutamate at toxic levels, invariably leads to ALS.
A faulty immune system that attacks its own normal cells can cause the death of nerve cells also triggering ALS. Nerve cells may also be destroyed by the collection and accumulation of abnormal forms of proteins in the cells, again triggering ALS.
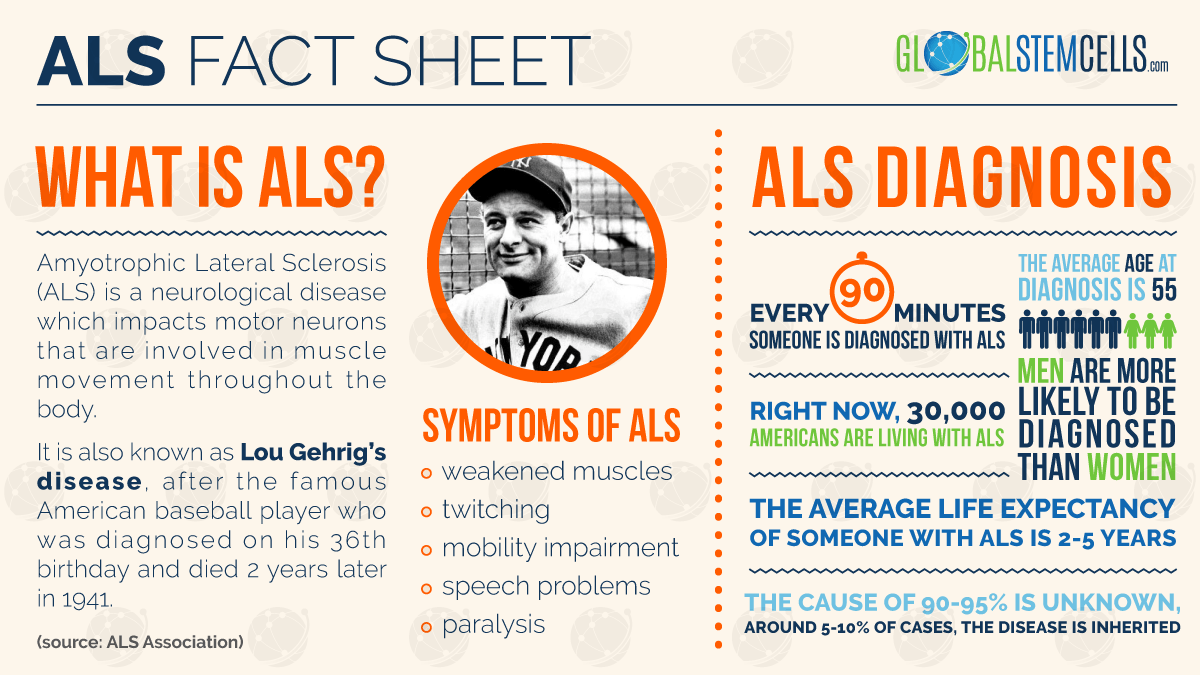
ALS Fact Sheet
Heredity, genetics, exposure to toxic substances and smoking are some of the primary risk factors. Treatment for ALS has centred mainly on relieving symptoms and improving the quality of life for patients. This is referred to as palliative care and relies heavily on the services of occupational, physical and speech therapists. Social workers, nutritionists and diverse caregivers also play a key role in this palliative care. Home care is also critical for the well being of the patient. Under normal circumstances this palliative care only serves to alleviate the patient’s suffering. The progression of ALS invariably leads to death.
Promising ALS Research
Now, however, stem cells bring new hope for persons suffering from this deadly disease. In a study conducted by the University of South Florida, researchers were able to use bone marrow stem cell transplants to repair damage to the blood-spinal cord barrier in mouse models of ALS. The studies in the mouse models demonstrated improved motor functions and nervous systems conditions. If this is successfully replicated in humans, the implications will be wide ranging as palliative care takes a secondary role and real healing takes place.
The blood-spinal cord barrier is crucial in the development of ALS. This barrier is located between the blood circulatory system and the central nervous system. Researchers in the University of South Florida’s Centre of Excellence for Aging and Brain Repair see the repair of this blood-spinal cord barrier as a critical step in using step cells in the eventual treatment of human beings. This particular study is particularly significant because it used mice with ALS unlike previous tests which used pre-symptomatic mice. Using mice with the actual condition approximates as closely as possible the conditions (and possible reactions) of a human being with the illness.
To conduct this study, the scientists began by using stem cells harvested from human bone marrow and intravenously transplanted these into mice modeling ALS and which were already displaying clear symptoms of the disease. Four weeks into the treatment the transplanted stem cells succeeded in differentiating and attaching to the vascular walls of many capillaries. This effectively triggered the process of blood-spinal cord barrier repair. The scientists also observed that the results from the mice which received higher doses of stem cells were noticeably enhanced.
Stem Cells and ALS
Stem cells have the ability to differentiate. This is the capability of the cells to develop into practically any cell type in the body. This makes them ideally suited for use in restoring function that had been lost through neurodegenerative disorders (such as ALS) or through injury. These particular stem cells differentiated into endothelial cells. These are cells which make up the inner lining of a blood vessel thereby providing a barrier between blood and spinal cord tissue.
The result of this treatment was to delay the progression of the disease which resulted in improved motor function and increased motor neuron cell survival.
H/T: Neuroscience News


 English
English